Squat Pivot Transfer

Let's talk about a highly useful, easily executed, underutilized transfer: THE SQUAT PIVOT
WHAT A SQUAT PIVOT TRANSFER IS NOT:
1. Stand pivot (with or without actual steps) with a walker: This is the preferred method for post-surgical to protect the limb, when there are weight bearing precautions or when a step or two needs to be made to get closer to the surface the transfer is being made to
2. Stand pivot (with or without actual steps) without a walker: If a seat is literally set up touching the seat your are leaving from, standing completely and turning or taking a step is likely not going to happen, not when you can just "pop" over (the Squat Pivot Transfer). This would most likely be used by someone who can stand, walk and needs to take a step or so to get to the surface they want to sit on. Or maybe they need to stretch out before sitting again.
3. Sliding board transfer: This transfer involves the armrest coming off and a patient sliding or boosting along
TAKE A LOOK AT THIS VIDEO TO SEE THE TASK OF SQUAT PIVOT:
TAKE A LOOK AT SQUAT PIVOT FROM BEHIND: Notice the trunk activity during the task. This is crucial and often not noted or observed during the assisting of or assessing of the task of Squat Pivot.
What do you see as Critical Steps for this transfer?
1. Ant Pelvic Tilt/Weight Transfer/Lift off: Just like sit- stand
2. Trunk LENGTHENING on the side the transfer is gong to with active trunk SHORTENING on the side the transfer is moving away from: this drives the pivot
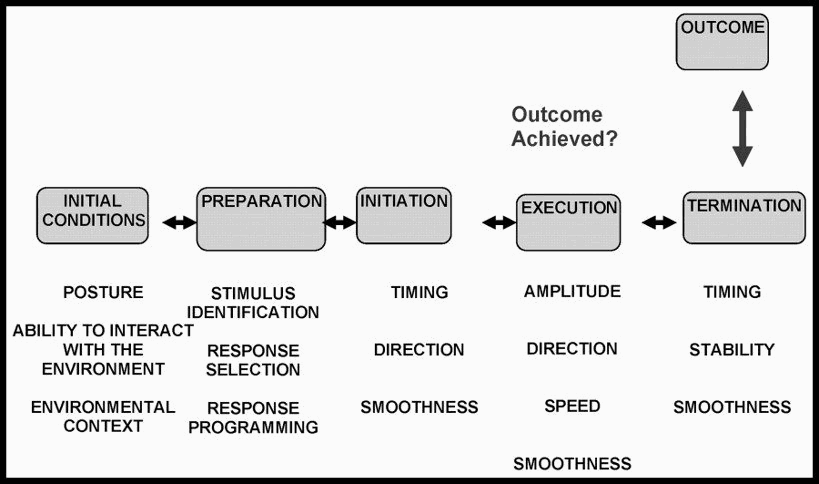
STEPS FOR TASK ANALYSIS:
1. Consider "normal" execution and basic required elements.
Normal Task Analysis form.docx
Remember your reference:
2. Hypothesize patient's ability
- Prior notes from PT/OT or nursing
- Conversation with patient/family
- Initial observation (what are the INITIAL CONDITIONS)
- Application of known health condition and co-morbidities on impact of necessary neurological, cognitive and musculoskeletal demands of the task- does this patient have a co-morbidity that necessitates the teaching a modified sit to stand for safety?
3. Prepare yourself for the needed level of assistance
- Now much assistance will the patient likely require? Do you need an additional person?
- Do you need to adjust the environment (for sit to stand- what about chair height)
4. Ask the patient to do the task: "Go ahead and have a seat in that chair" motioning to the seat you are indicating.
4. Observe the INITIATION. Compare it to "normal" and assess if it is effective. (if it is effective and appropriate, and needs no modifying, let it go)
- This is the most difficult part. Do nothing!!!!! Safely observe how the patient initiates the movement. See how the patient attempts to rise from the surface.
- Regarding the Critical Elements, ask yourself:
Is the patient getting sufficient anterior pelvic tilt
Is their weight adequately shifting from the seat to the feet
Is there lift off
Does the trunk actively (and head) shorten on the side the patient is moving FROM (transfer to the left, the right side shortens)
Is there sufficient length in the side toward the transferring side for the weight shift to happen
5. Provide assistance as needed to accomplish the task.
Know where to touch: your touch should facilitate the movement. Your movements should align with the needed movement pattern/direction for the task to enhance the success and not "get in the way" of the patient's attempt.
Your Input + the patient's effort = Success.
*** Do Not Correct on the 1st Attempt***
6. REPEAT the task.
This time, provide additional input to substitute for the impairment you hypothesized was limiting the patient's success.
Ask yourself: Did the task become 'easier", more successful, when I added this intentional input?
If so: Add it to your problem list
If not: move on to the next hypothesized impairment
Continue in this fashion until all possible impairments have been assessed.
RESULT: A list of impairments directly impacting the performance of sit to stand. These impairments will be the initial goals of your interventions
*There is an example of this process below following the lesson on assisting with various styles for STS
EXAMPLES OF ASSESSING/ASSISTING SQUAT PIVOT
As with other tasks, different therapists offer different approaches. Below you will see two videos with differing approaches. But, the intent is the same. To ASSESS the ability of the patient and lighten/tighten at the right moment to understand their initiation and execution of the task, while being ready to safely terminate the task with the appropriate amount of assistance.
COMMON ERRORS WHEN ASSESSING/ASSISTING SQUAT PIVOT TRANSFER:
- Crowding the patient. We must give the patient room to shift their weight anteriorly. Let the patient come to you, do not "go get them"
- Using momentum. Counting "1-2-3 Go!" is not appropriate for a patient where part of the assessment is the ability to initiate and when trying to observe and analyze their strategy for task execution. When you provide extrinsic cues, they are not showing you their ability to initiate and your handling for the "grab and go" for the "1-2-3" means YOU are deciding the technique.
- Making the patient look at the surface they are transferring to: This is contrary the the biomechanical advantage of the head hip relationship (see below)
- Not utilizing the head hip relationship: The head and hips move in opposite directions. This is a biomechanical principle that assists us in guiding and teaching movement.This task can not be performed well/safely without it. It must be cued and/or manually facilitated and definitely should be part of the training of the task. In sit- stand, the head moves forward and down as the hips lift up for lift off. In the Squat Pivot transfer, the head moves opposite the direction you are sending the hips (to the sitting surface) I think of it like how you manage a dolly with a refridgerator, or how you can't park the front and rear of a car into the parking spot at the same time.