Supine to Sit

Getting out of bed can be a very difficult task for some people following an orthopedic or neurological event. This section is looking at supine to sit: the process of coming up to sit on the edge of the bed from a supine position.
Log Rolling:
This is a common technique used when learning to ASSIST a patient with bed mobility. In the acute care setting, when assisting to do bed changes and hygiene, this is the preferred technique. However, when ASSESSING their strategy and ability to execute a preferred strategy this may not be ideal
When is it the best choice: When the patient has or has recently experienced an orthopedic injury or surgery which makes the task of supine to sit painful or impossible. Some examples include:
*abdominal surgery, ACDF, spinal surgery, wearing a cervical or lumbar brace, severe kyphosis with risk of fracture
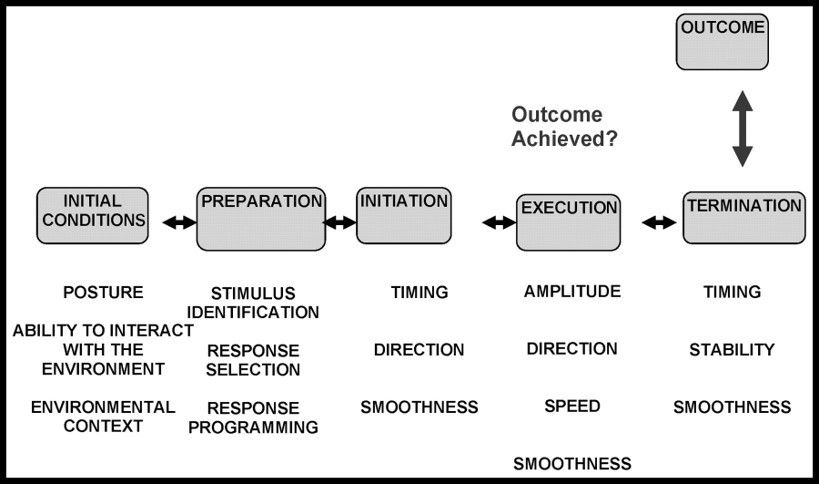
ASSESSMENT of a functional task includes the observation of the initiation and execution of the strategy the patient preferentially uses. During assessment, the goal is to see what the PATIENT can do and the approach that is most familiar, their pattern for the task. Restoring capacity for a familiar task will be less difficult for a patient with compromised motor control as compared to teaching a new, unfamiliar task pattern.
SUPINE TO SIT
STEPS FOR TASK ANALYSIS:
1. Consider "normal" execution and basic required elements.
Normal Task Analysis form.docx
Remember your reference:
2. Hypothesize patient's ability
- Prior notes from PT/OT or nursing
- Conversation with patient/family
- Initial observation (what are the INITIAL CONDITIONS)
- Application of known health condition and co-morbidities on impact of necessary neurological, cognitive and musculoskeletal demands of the task- does this patient have a co-morbidity that necessitates the teaching of log rolling for safety?
3. Prepare yourself for the needed level of assistance
- Now much assistance will the patient likely require? Do you need an additional person?
- Do you need to adjust the environment (for rolling- what about bed height)
4. Ask the patient to do the task: " Go ahead and sit up on the edge of the bed " (or: "Go ahead and lie down on the bed" for the reverse motion)
And... WAIT! Part of the assessment is the ability to initiate and being able to SEE HOW and WHERE they initiate the task form . This assists us in understanding their compensations and volitional access to movement and their preferential strategy.
4. Observe the INITIATION. Compare it to "normal" and assess if it is effective. (if it is effective and appropriate, and needs no modifying, let it go)
5. Provide assistance as needed to accomplish the task.
Know where to touch: your touch should facilitate the movement. Your movements should align with the needed movement pattern/direction for the task to enhance the success and not "get in the way" of the patient's attempt.
Your Input + the patient's effort = Success.
*** Do Not Correct on the 1st Attempt***
6. REPEAT the task.
This time, provide additional input to substitute for the impairment you hypothesized was limiting the patient's success.
Example: You think the patient is not able to complete cervical flexion/rotation against gravity, so you gently guide cervical rotation to see if it helps reduce the level of outside assistance for the task.
If so: Add it to your problem list
If not: move on to the next hypothesized impairment
Continue in this fashion until all possible impairments have been assessed.
RESULT: A list of impairments directly impacting the performance of rolling. These impairments will be the initial goals of your interventions.
ROLE OF OTHER ASSESSMENTS IN THE TASK ASSESSMENT?
We have other assessment tools to understand the impact of a health condition on the human body. Tools such as MMT or ROM assessment. The results of these tests will provide additional information to solidify your understanding of the true impairments impacting the task. For example: I note that the ROM in the neck for right rotation is limited and I know that most folks use rotation during rolling. I DO NOT want to put that impairment on my "recipe" list for interventions until I know it is a limiting factor. So the ROM assessment confirms a ROM limitations is present... but you still have to answer the questions "So What?". Meaning, does it impact function? Repeat the task with YOUR giving the missing rotation and see if the task improves, if so, it matters. If not, it likely does not matter and should not be added to your list of problems.
This is an important step so all positive findings (weak grip, kyphosis, asymmetrical pelvis) are not added to the treatment list unnecessarily.
Watch this video of a technique for assessing SUPINE to SIT (and reverse)
Point of Initiation for Supine to Sit: Cervical Flexion (followed by sequential upper trunk flexion then rotation)
- when the task is initiated and sequence of motor recruitment is appropriate, the action of the trunk rotators pulls the pelvis over and there is NOT as much LE hip flexion needed as it may seem. You do not have to be a 5/5 for supine to sit in the LE hip muscles.
COMMON ERRORS IN ASSESSING SUPINE-SIT
1. Assisting the patient (pulling them up) before they initiate. This is not assessment.
2. Getting under the shoulders and pulling up. The cervical flexion is key for this task and absence of it, biomechanically, significantly disrupts the ability to sequentially recruit the trunk muscles for flexion and rotation.
3. Dropping the legs off the side first. This biomechanically disadvantages the trunk muscles by placing them in a lengthened position.
4. Doing too much. Match the patient's needs. The need they have for assistance may be less and more through different phases of the task. "Lighten and Tighten" as needed to feel the variations in ability. Be willing to give the patient time to plan and recruit. There is valuable information for understanding their movement dysfunction when assessment is done intentionally and geared toward understanding where the patient is and is not successful through the stages of the task.
TIPS FOR OBESE PATIENTS:
The strategy of beginning the task with "Go ahead and sit up on the edge of the bed" is the best approach for this population as well. The task of supine - sit has a strong cervical flexion/upper trunk then rotation component. A large abdomen will bet in the way of this pattern of task completion being successful. Therefore, this population may have accommodated with a normal task variation including momentum, pulling with UE on the edge of the bed or side lying to sit.
WHAT IF MY PATIENT IS MAX ASSIST OR MORE?
The process of assessment of the task is the same no matter what the level of assistance is. And, you will not know what the level of assistance is until you do the above mentioned steps. Once you initiate the process, you will see the severe inability to initiate and execute the task and you will assign it a functional level (i.e. max assist)
SUGGESTED DOCUMENTATION:
Identification of a level of assistance is NOT an assessment of a functional task. Identifying the patient is NOT able to perform it independently is the beginning, not the end of a task assessment. Once you identify the patient requires assistance, then ask "why". This is where the test-retest approach is necessary. It'll guide you to understanding the "why". The information you gain from the task assessment is added to your functional level of assistance to complete the picture of the movement dysfunction.
EXAMPLES:
Supine-Sit: Min assist for cervical flexion
Supine - Sit: Max assist for cervical flexion, trunk flexion/rotation
Supine - Sit: Max assist for LE management
Supine - sit: Min assist for sitting balance at termination
WHY IS THIS IMPORTANT?
Read this statement:
"Supine - Sit: Mod assist"
You are now scheduled to treat this patient. They are mod assist for supine - sit and there is a goal for "Pt will be mod I for supine to sit by d/c". What will do do for treatment today? It is likely you will do something not related to the task (increase their leg strength or arm strength) OR you will need to do a re-assessment of the task.
Now, read this statement: (goal is still "Mod I for supine to sit by d/c")
"Supine - Sit: Mod assist for LE management" : where will you focus your treatment?
What about this one:
"Supine - sit: Mod assist for sitting balance at termination" : where will you focus your treatment?
See the difference? In the second set of scenarios, it is CLEAR the limiting factor for the task. To meet the stated goal, it is clear what needs to improve. The first example merely stated the level of functional assist- "mod assist". There is NO TREATMENT FOR MOD ASSIST. But in the second set, the "why" is identified and anyone (you, covering PT, PTA...) providing treatment would know the limiting impairment and be able to develop INTENTIONAL INTERVENTIONS which specifically target the unique limiting factors of the task for this patient. When we document the "why" the interventions are clear, consistent and targeted.
OTHER COMMONLY USED METHODS TO ENTER/EXIT BED:
1. Prone to stand
2. Crawling in
3. Momentum (LE into chest, then "pop" out)
4. Sidelying to stand and go
Not everyone stops in a sitting position prior to exiting bed. However, for most patients, this will be transition position until they have improved to a more independent state. These options, however, should be considered to be viable if a patient is able to complete safely. Do not "take away" their method because it makes you uncomfortable. Observe, and train for success as it will be their "go to" in the future. Only if it is not a viable option do you completely alter their strategy. NOTE: it is OK to tell your patient that 'for right now, crawling is not the best choice, let's try it this way until we can make your way safer" then include that strategy in your training. Salience is important for motor recovery!