Sit-to-Stand/Scooting

Sit to stand is the most functional task we have discussed thus far. This transitional phase is utilized in multiple settings, from multiple heights and correlates with independent living in the elderly. Think: getting up from the toilet, from a car, from a movie seat, from a park bench, from a curb, from the dining table, etc. Despite the variations there are basic elements of a sit to stand movement which remain constant.
From a biomechanical aspect, three phases of sit to stand exist: phase 1, weight shift; phase 2, transition; and phase 3, lift.
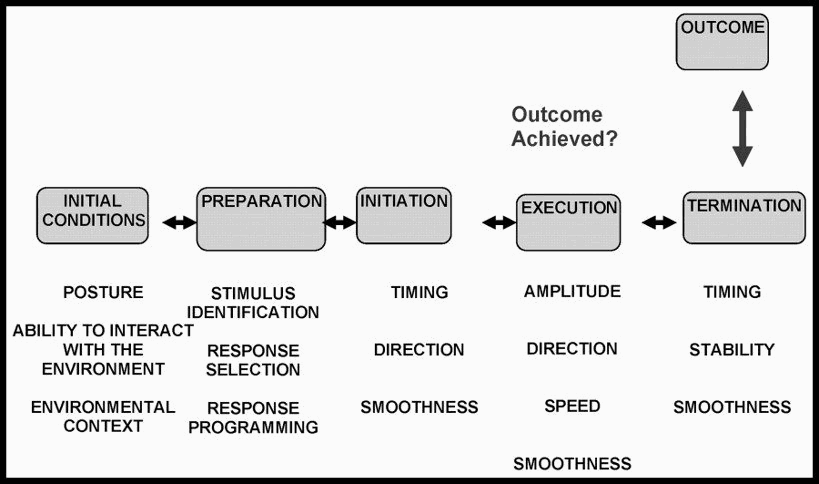
Where would you place these phases within the framework of our normal task analysis?
STEPS FOR TASK ANALYSIS:
1. Consider "normal" execution and basic required elements.
Normal Task Analysis form.docx
Remember your reference:
2. Hypothesize patient's ability
- Prior notes from PT/OT or nursing
- Conversation with patient/family
- Initial observation (what are the INITIAL CONDITIONS)
- Application of known health condition and co-morbidities on impact of necessary neurological, cognitive and musculoskeletal demands of the task- does this patient have a co-morbidity that necessitates the teaching a modified sit to stand for safety?
3. Prepare yourself for the needed level of assistance
- Now much assistance will the patient likely require? Do you need an additional person?
- Do you need to adjust the environment (for sit to stand- what about chair height)
4. Ask the patient to do the task: "Go ahead and stand up from the chair or bed" (or: "Go ahead and sit down on the bed or chair" for the reverse motion.
4. Observe the INITIATION. Compare it to "normal" and assess if it is effective. (if it is effective and appropriate, and needs no modifying, let it go)
- This is the most difficult part. Do nothing!!!!! Safely observe how the patient initiates the movement. See how the patient attempts to rise from the surface.
- Regarding the 3 phases, ask yourself: Is the patient in mid-line for a proper weight shift? Does the patient demonstrate correct biomechanics to un-weight the buttocks? Can the patient develop sufficient force for lift off?
5. Provide assistance as needed to accomplish the task.
Know where to touch: your touch should facilitate the movement. Your movements should align with the needed movement pattern/direction for the task to enhance the success and not "get in the way" of the patient's attempt.
Your Input + the patient's effort = Success.
*** Do Not Correct on the 1st Attempt***
6. REPEAT the task.
This time, provide additional input to substitute for the impairment you hypothesized was limiting the patient's success.
Ask yourself: Did the task become 'easier", more successful, when I added this intentional input?
If so: Add it to your problem list
If not: move on to the next hypothesized impairment
Continue in this fashion until all possible impairments have been assessed.
RESULT: A list of impairments directly impacting the performance of sit to stand. These impairments will be the initial goals of your interventions
*There is an example of this process below following the lesson on assisting with various styles for STS
HOW TO ASSIST and ASSESS THE TASK OF SIT -STAND
Let's get started with this task!
In the clinic, STS can be a challenging task for YOU and the patient.
This entire video is an assessment of her sit- stand. I assist, tighten/lighten to see where she needs assistance and where she doesn't, then attempt to test/re-test by providing manual and verbal cues to adjust her movement control. You can not do this, however, unless you work from the beginning and know where to put your hands and have a good understanding of what you are trying to accomplish (thus the task analysis)
Watch this video showing how to approach a min assist patient:
There are various methods to use for assisting/assessing the task of sit- stand. Which you choose depends on the patient's needs, your hypothesis of their strengths/weaknesses/capacity, YOUR height and the setting, to name a few.
This video shows variations for body positions to assist/assess this task:
This video shows an approach for a patient needing more assistance, perhaps moderate to maximal assistance:
TEST/ RE-TEST for patient needing more assistance (Step 6 of the Task Analysis)
Watch this example of test/ re-test: You think the patient is not able to complete forward weight sift over the base of support. You can provide input at the scapula and and facilitate anterior pelvic tilt to increase trunk flexion and create forward weight shift prior to lift off.
Here is a video clip for you:
SO, WHAT ABOUT THE ARMS? WHAT IS THEIR ROLE IN STS?
COMMON ERRORS OF THE PT WHEN ASSESSING/ASSISTING STS:
- Crowding the patient if facilitating from the front. We must give patient room for forward translation of femurs, for sustained forward trunk flexion, for head to move forward.
- Using momentum rather than weight shift to achieve lift off. Do NOT use "Ready? 1,2,3 stand up!" If we don't place a power demand on the patient, s/he will not learn to activate required extensors for the task. In addition, s/he will not learn to sequence the task appropriately. Part of assessment is initiation (its part of the task) we can not initiate for them, the value is in letting them initiate so we can examine their chosen strategy and its success.
- Insufficient limb flexion prior to lift off. It is common for patient with hip or knee impairments to "favor" them and decrease their use with reduced flexion positioning. (Keeping knees straighter and ankles in more plantarflexion). If a patient has insufficient hip, knee or ankle flexion, they won't stand successfully. Try it! Stand up with your hips, knees or ankles in relative extension.
- Mandating scooting to the edge and use of UE, versus assessing if those additional elements are needed FOR THIS patient and using them individually to maximize the patient's success.
- To scoot, or not the scoot? That is the question. We discussed the required elements for successful sit to stand and scooting was not one of them. Why is scooting not a required element for the sit to stand task? Try it! Sit down in a chair. Relax against the back of the chair. Really lounge. Stand up! How did you accomplish the task? Here's the real question.....did you scoot? Probably not. There are only a few conditions which require a person to scoot forward prior to standing up. If the patient is NOT impacted by the following conditions for normal sit to stand, we do not introduce an abnormal movement pattern of scooting to accomplish the goal of standing up.
- Here are barriers for sit to stand that may require scooting:
1. Obesity. If a person cannot sufficiently flex the trunk forward or attain anterior pelvic tilt, due to large abdominal size, they may need to scoot first.
2. Lack of strength and power. Due to frailty, post-operative conditions, impaired strength or ROM, a person may lack sufficient power to perform sit to stand task without scooting.
3. Pain. Trunk or limb movement in some, may create an increase in pain therefore limiting the amount of forward excursion required for standing. They may need to scoot.
Here is a video view of scooting:
Hand placement to facilitate scooting:
Objective tests and measures that directly assess sit to stand
1. 30 second chair stand test
2. 5 times sit to stand
3. Modified 30 second sit-to-stand
Objective tests that contain sit to stand elements
1. Berg Balance Scale
2. FIM
3. MiniBestest
4. Tinetti
5. TUG
ARTICLES RELATED TO SIT-STAND (not testable material)
Sit- Stand Changes in Stroke patients
Benefit of Facilitation in Sit to Stand